By Leroy Leo and Sriparna Roy
(Reuters) – Smaller rivals to UnitedHealth’s tech unit Change Healthcare say they are signing longer-term contracts with hospitals and other customers who had temporarily switched from the company after February’s cyberattack shut down the unit’s services.
The new contracts landed by Waystar and privately held Availity and Inovalon show a shift to healthcare practices signing deals with multiple service providers instead of relying on a single vendor, in what may be the first sign of needed change in an industry. Health tech experts said the move to more than one vendor is long overdue, but was hastened by the hack.
Change makes up only 1% of revenue at healthcare giant UnitedHealth but processes about 50% of medical claims in the U.S. for around 900,000 physicians, 33,000 pharmacies, 5,500 hospitals and 600 laboratories. About 1 in 3 U.S. patient records are processed in some way at Change, according to the company.
“The industry is realizing that the single point of failure is just too risky in the current environment,” Eron Kelly, president of Change’s smaller rival Inovalon, said.
FEBRUARY HACK
In the days and weeks after the Feb. 21 ransomware attack, many doctors and hospitals struggled to file claims, resorting to paper to verify insurance coverage as the electronic systems were taken offline. For months, many struggled to be paid.
The hack hurt people doing business directly with UnitedHealth, but many providers also realized they had indirect exposure through other software vendors. UnitedHealth estimates the hack’s cost at up to $2.45 billion this year.
Wall Street analysts and tech experts said it was difficult to quantify any changes in market share or if the market had increased, citing a lack of data.
Roger Connor, CEO of Optum Insight, the division that includes Change, said in an emailed statement that the company has brought back a “very secure” technology system that is resonating with customers.
“We’re not only trying to bring volume back into our current customers. We’re also working to bring new clients in,” said Connor.
KEEPING CUSTOMERS
Inovalon’s Kelly said after the hack, the company contracted with organizations whose ranks included about 344,000 separate providers, such as doctors, pharmacists, and nurse practitioners. That compares with more than 8 million providers nationally, which are counted using their unique national provider identification numbers, according to government data.
About 98% of those providers are now on long-term contracts, Kelly said.
Some “payers” – typically health insurers and other groups handling reimbursements to providers – who previously had exclusive contracts with Change, had also shifted, Kelly added.
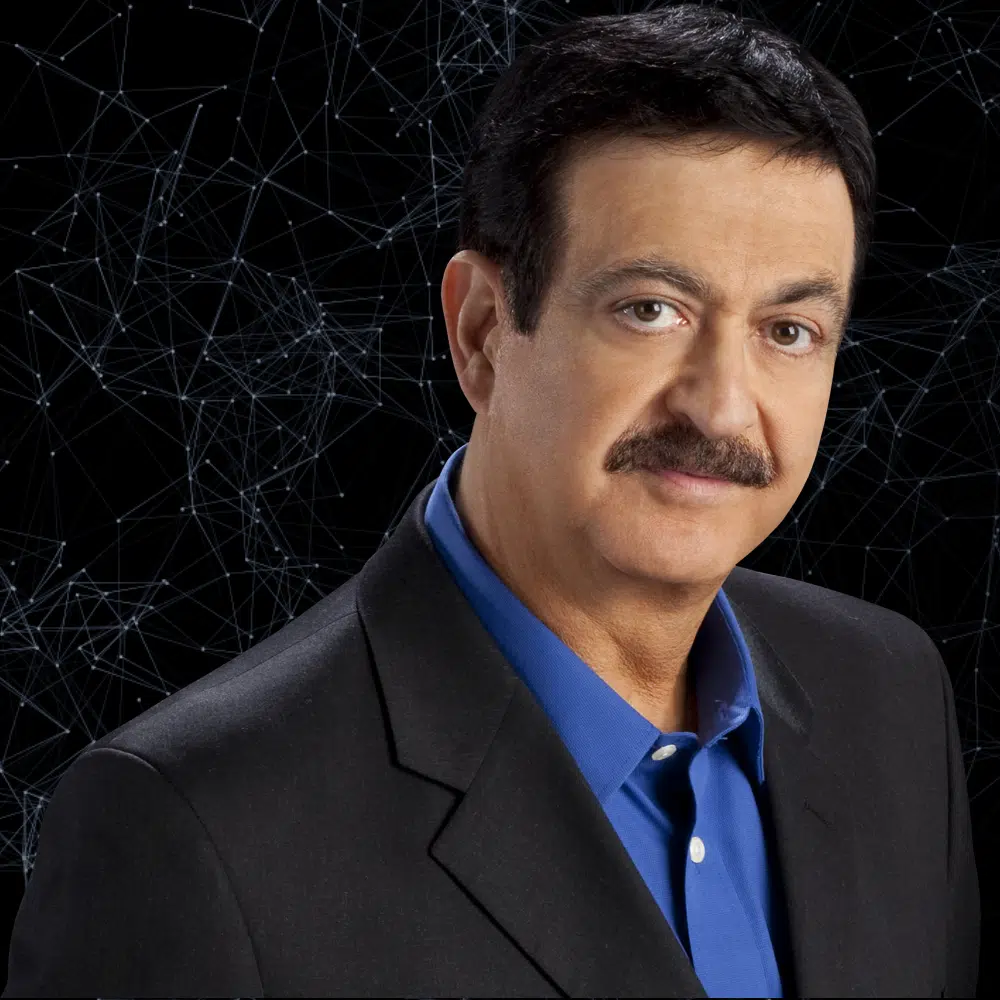
Availity, a firm backed by health insurer Elevance, launched Lifeline, a free, scaled down version of its services for claims processing, after the hack. The service helped process claims for over 300,000 providers such as doctors, hospitals and other medical practices across 120 health organizations, said CEO Russ Thomas.
Since the hack through mid-July, Lifeline helped with claims worth an estimated $315 billion, the company said.
Now, it is working to make the clients permanent.
“We are out meeting with the clients, sharing the full scope of what we can do for them, and fortunately, having some good success in converting to long-term clients,” said Thomas.
The company declined to disclose how many customers became permanent.
Recently-listed Waystar also sped up how quickly hospitals and doctors’ practices could switch to its software platform for managing their finances, allowing them to get up and running within 72 hours of signing a contract.
It also rapidly scaled up back-end operations to deal with more than 30,000 providers joining the company’s platform.
The company has said that most of its clients have signed standard contracts for two- and three-year terms.
ADDING VENDORS
Some providers of software for smaller, independent healthcare practices, such as privately-held Tebra’s billing program Kareo and TherapyNotes, used by mental health practices, are either leaving Change or adding an additional vendor.
Tebra had used Change for verifying patients’ insurance eligibility in its Kareo software, but has shifted about 99.7% of that traffic to other service providers, according to Tebra Chief Technology Officer Kyle Ryan.
About 10% of the company’s electronic claims volume had also moved through Change before the hack and that number is now down to 2%, Ryan said in e-mail.
Jeremy Wall, managing director at global strategy consulting firm Stax, said that providers are also likely adding more vendors than switching completely.
“What we have seen and heard from people in the market is that a pretty large portion of the people who moved over to another vendor have stayed over with that vendor,” Wall said.
(Reporting by Sriparna Roy and Leroy Leo in Bengaluru; Editing by Manas Mishra, Caroline Humer and Anna Driver)


Comments